Most of us have had a form of bacterial infection (or invasion) at some point in our lives where the doctor treating us prescribes us some antibiotics. We are all told to "finish", "complete" or "take all" of the prescribed antibiotics. Many of them stress that you need to take the full course or else risk not killing all of the disease-causing bacteria, allowing it to mutate and form a resistance to the treatment.
Although this may have appeared as sound judgment, it turns out this may never have been the case. Have we been told falsities about how to use antibiotics to overcome an infection in our body? Most likely, as new research is saying there is no evidence that this old theory about not finishing a course of antibiotics leads to antibiotic resistance. Finishing antibiotic treatments is likely producing greater antibiotic resistance.
The idea of antibiotics needing to be taken in full as prescribed or else it could create antibiotic resistance comes from the 1940s when antibiotics first started. In running out of penicillin for a patient, a clinic noticed the patient succumb to the infection again despite having improved while being treated. The idea of prolonging therapy to avoid treatment failure was adopted, but there was no evidence of antibiotics resistance.
They posited the idea of someone who had a streptococcal throat infection, not completing their antibiotics treatment, developing resistance, and then infecting someone like their wife who would get infected with the drug resistant form and die. Even though this ideas was accepted, after all these years Streptococcus pyogenes has never developed a resistance to penicillin.
This whole idea of not taking your full prescription antibiotics leading to antibiotic resistance, is not evidence-based and it turns out to be incorrect. The United Nations World Health Organization, and the US FDA, are still advising people to take the full prescription given by their doctor. They still think that if you don't take all your antibiotics, then you're not killing all of the disease causing bacteria, and allowing it to mutate into a resistance.
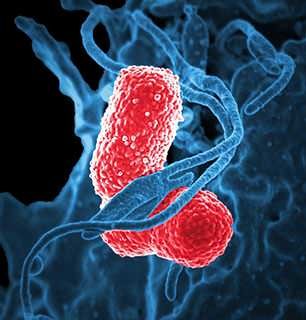
This new research dispels this fable by establishing links between treatment generation, effectiveness and drug resistance, finding no evidence that a shorter treatment is inferior or that it triggers antibiotic resistance. Whenever we take any antibiotic, sensitive microorganisms on our skin or in our gut are replaced by resistant species and strains that are ready to cause infection in the future. The longer we take antibiotics, the more exposure we have and the more real estate those resistant species will take up in our bodies.
The study urges policy makers, doctors and educators to stop advocating for the "full course treatment" of antibiotics. Peter Openshawm -- president of the British Society for Immunology -- agrees, saying that antibiotics might be better used to only reduce the bacterial burden to a level where the natural immune system is able to cope with the infection and fight it off. Not that there isn't a case for extended treatment, such as for slow-growing or dormant bacteria.
After all these years, the antibiotic resistance that is spreading in society and causing big problems of untreatable infections in hospitals might be traced to the spreading of this false idea by doctors and policymakers early on. Instead of making sure harmful bacteria were killed, taking all of the prescribed antibiotics was making bacteria more resistant to antibiotics, and less effective in the future. If we would have been using antibiotics to lighten the load on our natural immune system, maybe the antibiotics resistance issue wouldn't be so big.
Have your local hospitals had issues with antibacterial resistance?
Does taking antibiotics bother you?
Do you avoid taking antibiotics?
Do you take antibiotics regularly?
I avoid them as much as possible. It's been years since I've taken an antibiotic. I haven't had a cold in years either. Montreal hospitals have had issues with the spread of the c. difficile bacteria in the past. I hope we can overcome the bacterial resistant era we are in.
Thank you for your time and attention. Peace.
References:
http://www.telegraph.co.uk/science/2017/07/26/gps-must-stop-telling-patients-finish-course-antibiotics-say/
https://www.theguardian.com/society/2017/jul/26/rule-patients-must-finish-antibiotics-course-wrong-study-says
https://medicalxpress.com/news/2017-07-message-antibiotics-experts.html
http://www.bbc.com/news/health-40731465
http://www.bmj.com/content/358/bmj.j3418
If you appreciate and value the content, please consider:
Upvoting  , Sharing
, Sharing  or Reblogging
or Reblogging  below.
below.