
The Flu Vaccine: Only 10% Effective – Is it still worth it? | Health & Medications
During my previous blog posts I talked about Common infant conditions as well as the various Ages & Stages of Childhood development. However, one thing we did not yet touch upon was childhood health conditions and if you’re a parent or have been around children for any period of time then you know first-hand just how prevalent these illnesses can be, especially when children enter school. This year particularly seems to be no exception, as schools are shutting down across the county in the United States. In fact, schools in at least 12 states have been shut down so far! So what is causing all these schools to shut down? The flu!!
In fact, contrary to popular belief, apart from the elderly (Age 50 years old) young children are at the highest risk for developing the flu as you can see from the chart below.
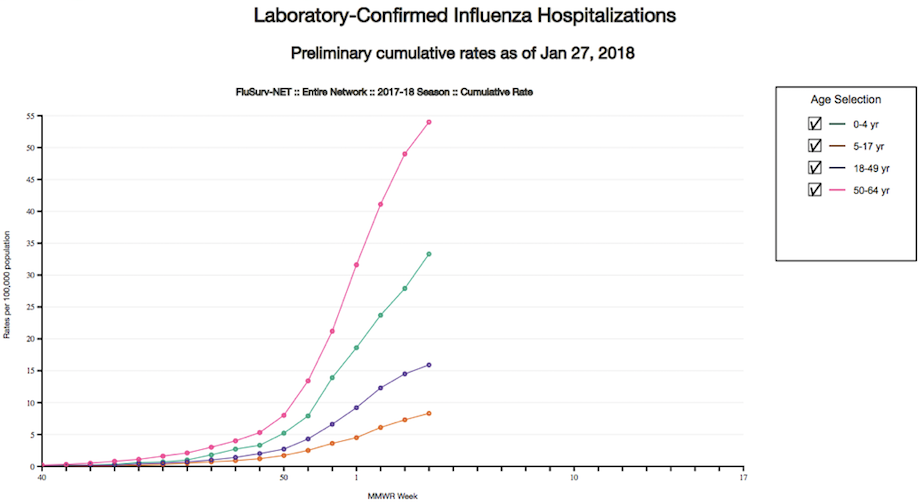
According to the Centers for Disease Control and Prevention (CDC), the 2017-18 flu season, is considered “widespread” in 49 states, which is the worst it’s been in over 15 years. In addition, there have been 53 reported pediatric deaths thus far! Aside from preventative measures like staying away from people who are sick, covering coughs and sneezes and frequent handwashing to help slow the spread of germs that cause respiratory illnesses, like the flu. The CDC recommends the flu shot each year as the primary method of prevention against the flu. However, there’s one major problem regarding this recommendation, which is the fact that recent studies have shown that the flu shot is only 10% effective. Put another way, if 100 in 1,000 unvaccinated people develop the flu, the number would drop to 90 in 1,000 among vaccinated people — as you can see this is a very small difference in flu risk between vaccinated and unvaccinated individuals.
Influenza A (H3N2) viruses predominated, and the preliminary estimate of vaccine effectiveness against influenza A (H3N2) is only 10%.
About the Flu
Most of us have heard about the flu, either from doctors, the news, family members, or even first-hand experience. Yet, what do you really know about the flu? How is it made? How do health officials determine which type of flu vaccine is made each year?
There are three different types of influenza virus – A, B, and C. Type A viruses infect humans and several types of animals, including birds, pigs, and horses. Type B influenza is normally found only in humans, and type C is mostly found in humans, but has also been found in pigs and dogs.
Type A influenza is classified into subtypes depending on which versions of two different proteins are present on the surface of the virus. These proteins are called hemagglutinin (HA) and neuraminidase (NA).
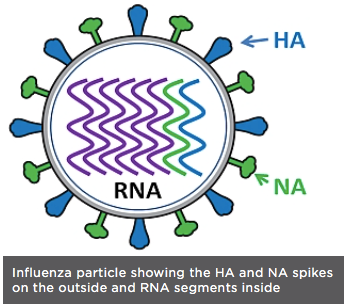
There are 17 different versions of HA and 10 different versions of NA. So, for example, a virus with version 1 of the HA protein and version 2 of the NA protein would be called influenza A subtype H1N2.
The HA protein allows the virus to stick to a cell, so that it can enter into a host cell and start the infection process (all viruses need to enter cells in order to make more copies of themselves). The NA protein is needed for the virus to exit the host cell, so that the new viruses that were made inside the host cell can go on to infect more cells. Because these proteins are present on the surface of the virus, they are “visible” to the human immune system.
How the Influenza Virus Changes from year to year
The influenza virus is one of the most changeable viruses known. There are two primary ways that the influenza virus changes – these are called antigenic drift and shift.
Drifting, or antigenic drift, is a gradual, continuous change that occurs when the virus makes small “mistakes” when copying its genetic information. This can result in a slight difference in the HA or NA proteins. Although the changes may be small, they may be significant enough so that the human immune system will no longer recognize and defend against the altered proteins. This is why you can repeatedly get the flu even if you’ve been vaccinated and why flu vaccines must be administered each year to combat the current circulating strains of the virus.
Shifting, or antigenic shift, is an abrupt, major change in the virus, which produces a new combination of the HA and NA proteins. These new influenza virus subtypes have not been seen in humans (or at least not for a very long time), and because they are so different from existing influenza viruses, people have very little protection against them. When this happens, and the newly created subtype can be transmitted easily from one person to another, a pandemic could occur.
How the production of the Flu vaccine could be contributing to its ineffectiveness
In September 2017, a study from Australia, demonstrated record-high laboratory-confirmed influenza notifications, high hospitalisation and mortality rates, particularly in New South Wales. The southern hemisphere influenza vaccine used in Australia is the same vaccine composition that is being used in the northern hemisphere (i.e., United States) for the 2017/18 influenza season. This was the first report of the ineffectiveness of this years flu vaccination.

In the U.S. most of the influenza-vaccine supply is currently produced from eggs. In addition, the composition of the 2017/18 flu vaccination is identical to that used in Australia, which helps to explain the increased prevalence of flu illnesses due to the low vaccine effectiveness against influenza A (H3N2) virus.
Another factor that may help to explain the low effectiveness of the influenza vaccine is due to the method used to produce them. In the United States, most influenza vaccine viruses are propagated in eggs. During the egg-based production process, the vaccine virus acquires amino acid changes that facilitate replication in eggs, notably changes in the hemagglutinin (HA) protein that mediates receptor binding. Since the influenza HA is the primary target of neutralizing antibodies, small modifications in this protein can cause antigenic changes in the virus and decrease vaccine effectiveness. Egg adaptation has been postulated to contribute to low vaccine effectiveness, particularly with influenza A (H3N2) viruses.

So to answer the overall question is it still worth it to get the flu shot? Well that depends on you. However, it does appear some may benefit particularly more than others, for instance children younger than 5 years and older adults with medical conditions. Since these individuals are at high risk not only for developing the flu but also more likely to be severely impacted by the flu, I recommend the flu shot to these particular high risk age groups. Although thats only my opinion on the topic. What are your thoughts?
Recent Posts:
- Common infant conditions | Health & Medications
- Ages & Stages of Childhood development | Health & Medications

