Unless you have been living in a cave for the last 10 years you must have heard of 3D-printing. Initially the first 3D-printers were simply harnessing conventional inkjet technology to deposit layers of materials following specifications of computer models to obtain 3D objects. As usual, technology progresses fast and advances in manufacturing techniques unlock new possibilities. The same is true also for 3D-printing.
Recently, there was a 3D bioprinting conference in Europe where scientists gathered to discuss what’s new in the field and how to use 3D-printing technologies in life sciences. One interesting idea was that put forth by Dr. Clive Roberts. He and his team have developed 3D printed tablets of different geometries to deliver drugs. They used beeswax as the drug carrier and mixed it with fenofibrate (an anti-colesterol drug), and used a special 3D-printing device to biofabricate tablets. Taking inspiration from nature, they made tablets with honeycomb-shaped cells that can be varied in size, thus controlling the surface area and consequently tune the rate of drug release (Kyobula et al., 2017).
Why is this important?
Let’s just say that the current way doctors administer drugs is less than optimal. The current system uses a “one dose fits all” kind of approach, this is problematic because patients of different gender, age, genetic makeup and “size” are given the same pills or tablets (Xie & Frueh, 2005). The problem is that the factors that I mentioned above influence also the efficacy of drugs (Meyer, Zanger, & Schwab, 2013). In an ideal world each patient should receive a custom prescription tailored for his condition. Until few years ago, we just did not have the technology to do this but with the recent advances in 3D-bioprinting it could become relatively easy for a doctor to print a custom tablet for his patients relatively inexpensively (take into account that drugs could be 3D-printed on demand, thus limiting the amount of drugs that expire because not used on time). Over time this option could prove to be extremely useful especially in light of the fact that with the aging population, we are also seeing an increase in the amount of medicines that each patient has to take (Hajjar, Cafiero, & Hanlon, 2007; Kennedy et al., 2014).
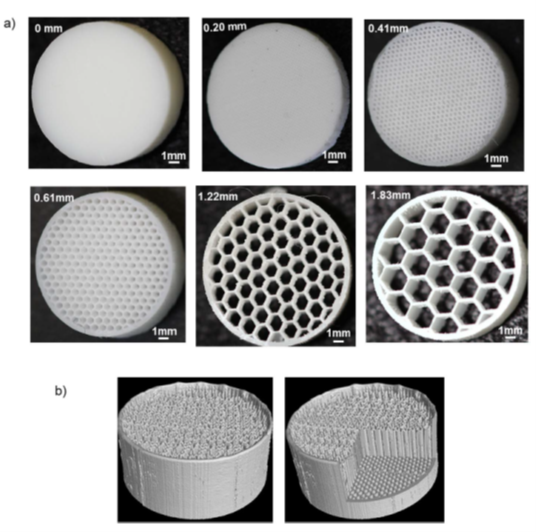
3D-printed custom tablets. Image from Reference (Kyobula et al., 2017).
Printing custom tablets may also increase the efficacy of a therapy while limiting the possible side effects due to wrong dosage or interactions with other drugs. A doctor in fact, could even modify the dosage of a drug based on how well the patient is responding or also considering eventual interactions with other drugs that the patient is taking.
As technology advances we could also learn to design tablets capable of releasing drugs in a controlled manner for prolonged period of time, possibly decreasing the frequency at which we need to take medications. Probably today this sounds too far ahead but I guess that in a few years this will most likely become a common practice, at least considering our current technology this is already very feasible to implement.
References
- Hajjar, E. R., Cafiero, A. C., & Hanlon, J. T. (2007). Polypharmacy in elderly patients. The American Journal of Geriatric Pharmacotherapy, 5(4), 345–351. https://doi.org/10.1016/j.amjopharm.2007.12.002
- Kennedy, B. K., Berger, S. L., Brunet, A., Campisi, J., Cuervo, A. M., Epel, E. S., … Sierra, F. (2014). Geroscience: Linking Aging to Chronic Disease. Cell, 159(4), 709–713. https://doi.org/10.1016/j.cell.2014.10.039
- Kyobula, M., Adedeji, A., Alexander, M. R., Saleh, E., Wildman, R., Ashcroft, I., … Roberts, C. J. (2017). 3D inkjet printing of tablets exploiting bespoke complex geometries for controlled and tuneable drug release. Journal of Controlled Release : Official Journal of the Controlled Release Society, 261, 207–215. https://doi.org/10.1016/j.jconrel.2017.06.025
- Meyer, U. A., Zanger, U. M., & Schwab, M. (2013). Omics and drug response. Annual Review of Pharmacology and Toxicology, 53, 475–502. https://doi.org/10.1146/annurev-pharmtox-010510-100502
- Xie, H.-G., & Frueh, F. W. (2005). Pharmacogenomics steps toward personalized medicine. Personalized Medicine, 2(4), 325–337. https://doi.org/10.2217/17410541.2.4.325

