G'day team,

Image source
So-called 'Super Bugs' have received a lot of media attention in the last few years but, in their usual fashion, the media outlets have mostly glossed over or miss-reported the details that underpin the problem. So today I thought I’d have a chat about what ‘Super Bugs’ are, why they’re such a threat and what’s being done to combat them.
What is a Super Bug
In a word...
Evolution
As with any plant or animal, bacteria are also constantly undergoing an evolutionary arms race to survive and prosper. The difference with bacteria is that they replicate at blindingly fast speeds (sometimes up to once every twenty minutes), and a little trick called horizontal gene transfer (think your mate giving you his blue eyes and 6 ft stature by shaking your hand) bacteria are actually far more effective at evolving than, say, a mouse, human or apple tree.
In the golden age of antibiotics, after WWII, the indiscriminate use of antibiotics such as penicillin provided a strong selective pressure for bacteria. In short, bacteria who were resistant to the antibiotic had a large advantage, and as such, they were selected for. To understand this better it’s easiest if we use an example.
Let’s say you've got pneumonia (an infection in the lungs). You have a colony of 1000 bacteria in your lungs but only 3 are able to survive high doses of penicillin. When your doctor, in an effort to save your life, gives you penicillin 997 bacteria die. Unfortunately, the 3 bacteria which survive begin to replicate and soon you've 1000 bacteria again, but this time all 1000 are resistant to penicillin.
And this, in a nutshell, is how antibiotic resistance develops. When those penicillin-resistant bacteria start to spread (through coughing, sneezing or saliva) to other people then all of a sudden we can no longer rely on penicillin and must use new drugs in order to eliminate infections.
The problem gets worse
Unfortunately, our troubles don’t end here.
As our reliance on antibiotics lead to their widespread and indiscriminate use (or overuse) the spread of antibiotic-resistant strains of bacteria followed suit. No sooner had a universities or pharmaceutical company developed a new class of antibiotics than we’d hear cases of resistant bacteria.
Soon we had strains we simply could not combat.
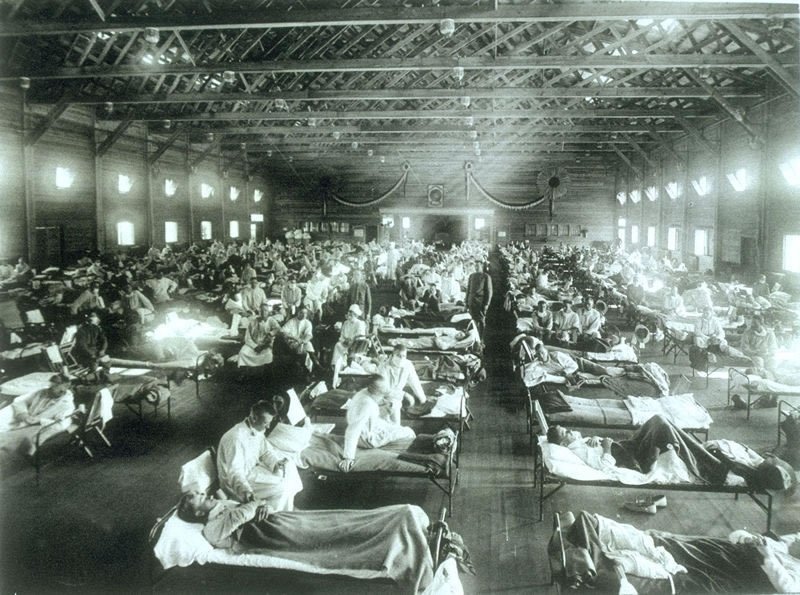
Hospitals, institutions which harbour those most vulnerable to infection, became hotspots for the spread of antibiotic resistance. Treating infections in an environment full of people who are especially vulnerable to infections (young, old, sick, pregnant and immunocompromised), has some quite obvious flaws.
Potential outcomes
So how big is this problem?
Unfortunately, it’s really big.
Before the time of antibiotics any simple infection could kill, and if we don’t overcome this issue before it overcomes all our antibiotics then we may be back in this age again.
If a heavily populated country, such as China, were to face a local outbreak of an aggressive bacterial infection resistant to our antibiotics then spread would be both far reaching and rapid. In 1918 the Spanish Flu wiped out about 3% of the world population. That was without travel by plane, without cities of 15 million people and without a globally interconnected world. Even if we had another pandemic the same as the Spanish Flu, 3% of the global population now is 228 million people or four to five times more than WW2.
Fighting the Problem
This was originally what I’d planned to write about, but without introducing the topic first I didn’t want my post to be overlooked for lack of understanding of the issue. A more detailed analysis will follow!
Combating antibiotic resistance has been a major global health challenge for decades now. But there are major political and technical drawbacks. For starters the issue is not a flashy one, it can’t be paraded in front of the media and no-one will ever win an election for their dedication to antibiotic resistance, so it gets very little funding. This being said, major health organisations have been putting significant pressure on governments around the world to help address the issue, so progress has been made. There are a number of major ways we can do this including:
Develop new drugs – this is the obvious solution, but the production of new classes of antibiotics has been slowing for decades and we’re close to a stand-still. Most new antibiotics that come out are re-makes of older drugs with little or no benefits over the original.
Antibiotic stewardship – one of the least exciting but most effective measures against antibiotic resistance is to really scrutinize when and where antibiotics are being used. Working together public health researchers, pharmacists, doctors and epidemiologists have been able to create guidelines for when antibiotics are really needed, and which ones can be used. This reduces our dependence on antibiotic use and decreases the chances of antibiotic-resistant strains of bacteria from developing in the first place.
Education in the third world – a lot of the worst cases of antibiotic over-use come from third world nations where access to antibiotics is easy, but access to health professionals to inform of their proper use is hard. By increasing funding and support for third world nations we decrease the chances of antibiotic-resistant bacteria developing in developing nations where they’re easily able to spread.
Healthcare hygiene – anyone with any healthcare training will tell you how much educators and hospital admin go on and on about hygiene. There are the five moments of hand hygiene (the stages when a doctor, nurse or other practitioner must wash their hands). There are sterile fields for basic procedures such as drawing blood and scrubbing down before every routine surgeries. And despite how tedious this is it is the healthcare initiative that may have saved more lives than even antibiotics and vaccines (feel free to argue this!). If antibiotic-resistant bacteria do develop, but are unable to spread from host to host, then they will not be able to enter the community and will inevitably perish within (or with) the host.
Image source
That’s it
So that’s a basic overview of so called super bugs. I’ll be writing a more detailed piece on the complex political, economic and scientific issues that have thus far prevented any big wins against antibiotic resistance, so keep watching my blog for that too!
Thanks team
-tfc
My Recent Posts
Hi, I'm Tom! (My life of medicine, science and fantasy)
Hydatidiform Mole – When Pregnancy Goes Wrong
Tags - Top 20 Profitable, Engaging and Popular tags
New Years Resolutions - How to set goals, and achieve them